About Me
My name is Brian Fox, and I am a manual therapist and strength coach. My specialty is using the unique skillset of a manual practitioner concurrently with that of strength science to help individuals achieve new and lasting levels of performance.
I have been in the industry since 2001, but my career took a turn onto the path of the Functional Range System in 2015. Some friends and colleagues and I took the FRC course with Dr. Spina in San Francisco, where I got hooked. From there, as a manual therapist, I took my first Functional Range Release course with Dr. Spina up in Oregon. The second FR course I took was lower extremity with Dr. Chivers in Toronto. Finally, I took the final FR spine course, again with Dr. Chivers, and it is also where I met John, as it was his final FR course as well.
I reconnected with John shortly after at the second course ever taught for the Functional Range Assessment in Austin, Texas, with Dr. Chivers and Mike Ranfone.
I began educating myself and using the Westside methods of strength training science about ten years ago, culminating in what I do today: strength training with a clinical lens.
Client Background:
Toward the end of 2024, I noticed a colleague of mine having an odd gate as he walked through the gym. He looked like that old Sasquatch video from back in the day. His knees were bent, and he had a noticeable lumbering walk as he cruised the gym floor.
I stopped him to ask him about his wonky walk, and we got to chatting further.
This person is a long-distance runner but by no means what we would call a “trained athlete.” His training up to this point consisted mostly of running and muscle-based training. He had done no prior connective tissue or joint training with his running and lifting.
This individual ruptured his Achilles and underwent surgery after he was performing an agility drill and changing direction. POP! The tendon did not have the requisite behaviors and abilities to absorb and dissipate forces during that task, resulting in a reactive strength injury and the tissue yielding.
Given Absolute’s updated definition of reactive strength, we know this to be on the bottom-up biological side of reactive strength rather than a neurological top-down issue, as it is not an output issue.
More from this original meeting.
Point A: Initial Assessment and Diagnostics
Obviously, with this injury and the history, there were a lot of different findings. However, the one finding that the client and I both found fascinating was the stiffness in the tendon.
This finding stood out and was intriguing because tendons have a stiffness and a compliant component. A “tendon is a variable mechanical tissue”; towards the bony attachment, the tendon is stiff, compared to where the tendon blends into the muscle, where it is more flexible and compliant (or should be).
His assessment revealed that the tendon was tremendously stiff, so stiff that it prevented any length and tension from traveling upward into the calf and soleus muscles. The muscles were completely soft and had no tension in/through them.
These findings reveal how the bottom-up biological component of reactive strength can affect the top-down component of reactive strength by disallowing the ability for length and force transmission to signal to the nervous system to contract muscle tissue. Oddly, there was no neurological tightness in the calf?!
These findings reveal the various siloes rather than being a functioning network. These findings made it clear where we needed to intervene. We needed to reestablish the neural network and the bottom-up biological components of the network. Those being connective tissue architecture, behavioral qualities of the architecture, and teaching the nervous system how to coordinate and self-organize those things again.
Functional Range Release + Functional Palpation Findings
The thickness of the affected Achilles is nearly twice the width of his other side.
The quality of the connective tissue of the Achilles tendon;
fibrotic and disorganized
scarring and lumps within the tissue.
Too much stiffness in the Achilles affecting tissue behavior
Inability to lengthen
Inability to transmit forces
No neurological tightness in the calf tissues
Achilles tendinosis is the inability of the connective tissue to transmit and dissipate forces. This leads to tissue breakdown and disorganization of the architecture, as well as loss of the behavioral ability to stretch.
Roadmap —> Point B: A Conjugate Strategy
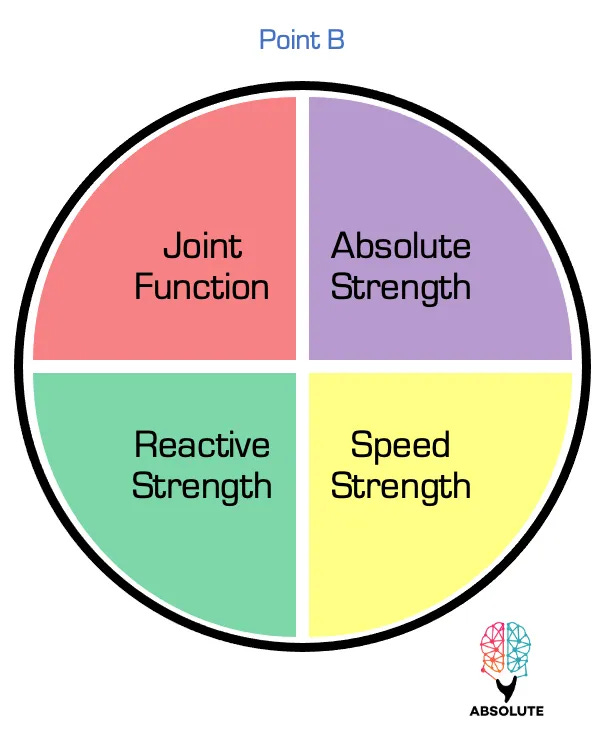
Managing different elements of Point B simultaneously: Joint Function and Reactive Strength.
Managing Joint Function
As a result of improving connective tissue architecture and changing behaviors of the architecture, i.e., length, we allow the nervous system to discover and connect to muscles and explore three-dimensional space, improving the central nervous system’s (CNS) map of space using controlled articular rotations (CARs)
This is a further example of how the bottom-up biological components of reactive strength affect the top-down components and the nervous system and the neurological network.
Managing Top-Down Behavior
Isometric Ramping (ISOr) and engaging specific muscle tissue
PIMAs (Pushing Isometric Muscle Actions)
Are we able to perform positional isometrics with these tissues? Are we able to produce force at length (PAILs or Progressive Angular Isometric Loads)
Reactivity
Can this happen rapidly?
Managing Reactive Strength
Connective Tissue Architecture (CTA)
Improving quality and quantity > order/organization
Behaviors
Length
Can the tissue achieve length, and can the client/patient experience that as well?
CT Load-Bearing Capacity (LBC)
Can the tissue absorb and dissipate forces at and too length?
Stiffness/compliance
Is the tendon behaving optimally for the individual's demands, ensuring the correct blend of stiffness and compliance? We began with a hard no!
Reactivity
Can the tissue and CNS harmonize to absorb, dissipate, decelerate, and rapidly change direction or pop?
Given the nature of this injury, our clinical focus is on the left side of the pie chart, with a priority on the biological bottom-up component of reactive strength.
This helps to clarify our constraints and intent with treatment and training inputs.
HOW: Using training as a mechanism and manual assessments to push adaptation and drive recovery.
A Conjugate training strategy is used in both the clinical and training setting. Training multiple ecologies and capacities simultaneously over time.
Training includes a Bulgarian-style method, which involves training at a stimulating intensity multiple times daily. Keep in mind that we are trying to stimulate connective tissue architecture and behaviors, which necessitate specific stimulating intensities.
Training and treatments also require multiple feedback mechanisms to determine how to logically and successively produce training over time and to achieve Point B.
Reassessments, training results, and client feedback.
Using the LLP and IIC as feedback mechanisms in conjunction with client feedback.
The Roadmap: Conjugate Sequencing System
The end goal of Point B, or my client’s goal to have “a healthy and functional” Achilles tendon, and return to normal activities. But we can’t focus on that. Looking up at the summit of Everest is daunting. We have to take it one step at a time and make each step count along the way.
Rather than focusing on getting from A to Z, we need to focus on the processes that lie between — B through Y.
Establish Point A → B-Y (process) → Z (multiple Point Bs on our journey to the apex of Point B)
The end result feeds into and becomes the starting point for the next series of processes and results, and so forth.
The process is the roadmap, and are the strategies employed along the way.
This is the Conjugate Sequencing System. It involves breaking down a goal into smaller tasks, completing them in a logical and sequential manner, performing them well, gaining feedback, and moving on to the next task. This process involves completing each rep, each input, each training session, each day of multiple training sessions, and each week, accumulating marginal gains over time.
Roadmap Examples
September
Because he was in the non-acute phase of his injury and surgery, and because of our assessment findings, we knew right where to begin our treatment and training journey, using the LLP and IIC as our navigators.
This initial training was designed to help him get used to being uncomfortable doing this type of training work in a safe environment. As a practitioner, I will always ensure my client’s safety, and as a coach, I’ll help you through the discomfort.
Block 1: Functional Range Release (FRR) + ISOramping (ISOr) + CT Architecture + Positional ISOm + HIMAs (Holding Isometrics) + CARs
FRR on scar site
ISOr calf tissue
HIMA & PIMA (Holding and Pushing Isometrics) contractions for CT architecture and neurology
CARs
(Video) Internal-Based Training > in the zone of ankle dorsiflexion > incline board
2-minute stretch
HIMA contractions in a 15:1 ratio x60s > up on two down hold on one
Very low effort and intensity. We even used a crutch-type assist to limit the load.
Ankle CARs
October
Verbal check-ins and reassessments act as feedback to help determine where to push our training to progress the stimuli.
Reassessment showed that the tissue's behavioral ability to lengthen and provide a stretching sensation in the affected tissue was evident. Further, length and tension were able to propagate up into the calf/lower leg musculature. Because of this, his ankle mobility improved as well (joint function).
This involved low-level static loading (stretching) and more HIMAs, only this time, we incorporated a deeper layer of tissue by targeting the soleus muscle. We also added in level 2 CARs to stimulate the plantar “stuff“ of the foot whilst getting intrinsic foot work in.
Block 2:
1-3 were completed without stopping.
Gastroc stretch x45s
Soleus stretch x45s
Repeated efforts with a hold at the top (ISOr) [Video]
Level 2 CARs > clenching a towel with the toes [Video]
November
We continued to follow the heuristic of a 2:1 static-to-dynamic ratio for the connective tissue architecture. Since our training’s main priority is biological in nature, we chose to progress along the LLP but stayed on the biological end of the IIC, keeping our efforts and intensities at or below 80%.
Being a reactive strength injury, we set forth with the intent to introduce velocity and reactivity.
Feedback and reassessment:
The positive feedback (adaptations) from the previous block of training indicated that we could use other components of the LLP and IIC. For example, since the ability to work at length has been established, we now want to work at length and from length (change of direction and rate of force development).
Block 3:
1-4 were done without stopping.
Static stretch x2min
Concentric calf raise with 3sec hold at the top
Eccentric with a 3sec hold at the bottom
Rapid change of direction —> 2
Ankle CARs w/ orange band resistance
December
We wanted to progress the reactive strength inputs while still using oscillations, keeping in mind resonance and ballistics. As an engineer, these concepts resonated with him.
Since these training concepts are novel to my client, when he performed the oscillations, I wanted to ensure that he was the oscillator. I wanted him to be in control of the frequency and rhythm of the dynamic resistance, with his tissue setting the pace before letting the load determine. His future training would involve introducing more randomness and allowing his “stuff” to self-organize.
Here we also experimented with two different band tensions for the oscillating loads. I used orange band tension to elicit a longer and slower wave, mimicking our training from the previous block. The red band tension was stiffer and shorter, making the oscillations faster. So, depending on the behavior we wanted in the tissue, we extracted from the band and load behavior.
Block 4:
Here is an example of the red-band oscillations on the slant board.
Present
I mentioned this element in the beginning. I wanted to emphasize where and how he got injured—jogging backward and trying to change directions. This also showed the value of the LLP and the IIC as feedback mechanisms to provide the confidence to execute this training.
To this point, we have created better architecture and better joint function and have not only created but observed behavioral traits in the tissue. However, this was all fear-based, not performance-based.
In this training block, we targeted the medial and lateral aspects of the Achilles by doing inversion and eversion on the slant board. We used similar inputs from previous blocks, just changing the ankle position slightly to avoid accommodation.
Block 5
Here is a video with the eccentric band exercise to train in a similar scenario in which he got injured.




This was a fantastic case study Brian. Thanks for the discussing and awesome post. Lots of great insights here.